Strabismus is a constant or intermittent deviation of the eye’s axis of vision from the point of fixation, leading to impaired binocular vision.
 Strabismus manifests itself as an external defect – deviation of the eye / eyes towards the nose or temple, up or down. In addition, a patient with strabismus may experience double vision, dizziness and headache, decreased vision, amblyopia. Diagnosis of strabismus is carried out by ophthalmological methods (visual acuity test, biomicroscopy, perimetry, ophthalmoscopy, skiascopy, refractometry, biometric examination of the eye, etc.), including neurological examination. Treatment of strabismus is carried out by spectacle or contact correction, hardware procedures, pleoptic, orthooptic and diploptic methods, surgical correction.
Strabismus manifests itself as an external defect – deviation of the eye / eyes towards the nose or temple, up or down. In addition, a patient with strabismus may experience double vision, dizziness and headache, decreased vision, amblyopia. Diagnosis of strabismus is carried out by ophthalmological methods (visual acuity test, biomicroscopy, perimetry, ophthalmoscopy, skiascopy, refractometry, biometric examination of the eye, etc.), including neurological examination. Treatment of strabismus is carried out by spectacle or contact correction, hardware procedures, pleoptic, orthooptic and diploptic methods, surgical correction.
In pediatric ophthalmology, strabismus (heterotropia) is observed in 1.5-3% of children, almost evenly among girls and boys. As a rule, strabismus occurs at the age of 2-3 years, when the joint work of the eyes develops; however, congenital strabismus may also occur.
Strabismus is not only a cosmetic defect. This disease leads to disruption of the functioning of almost all parts of the visual analyzer and may be accompanied by numerous visual impairments. Deviation from the central axis of the location of one or both eyes leads to the fact that the axes do not intersect on a fixed object. At the same time, in the visual centers of the cerebral cortex, monocular images viewed separately by the left and right eyes do not merge into one visual image, and a binary image of the object appears. To protect against double vision, the central nervous system over time suppresses signals from the squinting eye, resulting in amblyopia, a functional decrease in vision in which strabismus is almost or completely absent from the process of vision. If left untreated in children, about 50% of children develop amblyopia and vision deteriorates.
In addition, strabismus negatively affects the formation of the psyche, contributes to the development of isolation, negativism, excitability, limits the choice of profession and sphere of human activity.
Strabismus classification
According to the timing of occurrence, congenital (infantile – present at birth or develop in the first 6 months) and acquired (usually develop up to 3 years) strabismus are distinguished.
According to the stability of the deviation of the eyes, periodic and permanent strabismus are distinguished.
If we consider a slanting eye, then strabismus can be unilateral (monolateral) and variable (alternating) – with the latter, one or another eye is deviated, respectively.
According to the degree of severity, latent (heterophoria), compensated (detected only during an ophthalmological examination), subcompensated (occurs only when control is weakened) and decompensated (uncontrolled) strabismus are distinguished.
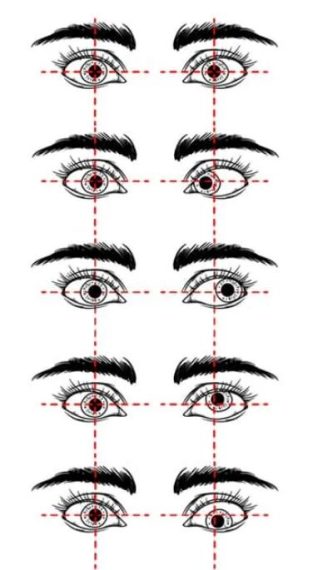
Depending on the direction of deviation of the squinting eye, there are horizontal, vertical and mixed strabismus.
- Horizontal strabismus can be convergent (esotropia, convergent strabismus – in this case, the squinting eye deviates towards the nose) and divergent (exotropia, divergent strabismus – the squinting eye deviates towards the temple).
- With vertical strabismus, two forms are also distinguished: the deviation of the eye up (hypertropia) and down (hypotropia).
- In some cases, there is cyclotropia – torsion heterotropia, deviating to the vertical meridian of the temple (excyclotropia) or nose (encyclotropia).
From the point of view of the causes of occurrence, concomitant and paralytic concomitant strabismus are distinguished. In 70-80% of cases, concomitant strabismus will be converging, and in 15-20% – receding. Torsion and vertical deviations are observed, as a rule, with paralytic strabismus.

With concomitant strabismus, the movement of the eyeballs in different directions is preserved in full, diplopia is not observed, and there is a violation of binocular vision. Associated strabismus may be accommodative, partially accommodative, or non-accommodative.
Accommodative accompanying strabismus most often develops at the age of 2.5-3 years and is due to the presence of moderate and severe hypermetropia, myopia, astigmatism. In this case, the use of corrective glasses or contact lenses, as well as hardware treatment, will help restore the symmetrical position of the eyes.
Symptoms of partially accommodative and non-accommodative strabismus are observed in children 1-2 years old. The refractive error in these forms of strabismus is not the only cause of heterotropia, so surgery is required to restore the position of the eyeballs.
The development of paralytic strabismus is associated with damage or paralysis of the motor muscles of the eye due to pathological processes in the muscles, nerves or in the brain itself. With paralytic strabismus, the mobility of the squinting eye is limited in the direction of the damaged muscles, diplopia occurs and binocular vision is impaired.
Causes of strabismus
The causes of congenital (infantile) strabismus include:
- The presence of heterotropia in a family history – the presence of heterotropia in close relatives;
- Genetic disorders (Cruzon’s syndrome, Down’s syndrome);
- Teratogenic effects of certain medications, drugs and alcohol on the fetus;
- Premature birth and low birth weight baby;
- Cerebral palsy, hydrocephalus, congenital eye defects (congenital cataract).
The development of acquired strabismus can occur in an acute form or gradually. Causes of secondary concomitant strabismus in children:
- Amitropia (astigmatism, farsightedness, myopia) – in this case, with myopia, converging is often formed, and with farsightedness, divergent strabismus;
- Stress;
- High eyestrain;
- Common diseases accompanied by high fever (juvenile rheumatoid arthritis), childhood infections (measles, scarlet fever, diphtheria, influenza);
- Mental trauma (fear).
At an older age, including in adults, strabismus can develop against the background of acquired cataracts, leukoma, optic nerve atrophy, retinal detachment, and macular degeneration.
Risk factors for developing paralytic paralysis:
- Tumors (retinoblastoma);
- Traumatic brain injury;
- Paralysis of the cranial nerves;
- Neuroinfections (meningitis, encephalitis);
- Stroke;
- Fractures of the wall and bottom of the eyeball;
- Multiple sclerosis, myasthenia gravis.
Symptoms of strabismus
The asymmetric location of the iris and pupil of the eye in relation to the orbit are objective signs of any form of strabismus. In other words, the asymmetrical location of the cornea relative to the corner and edges of the eyelid.
With paralytic strabismus, the mobility of the deviated eye to the paralyzed muscle is limited or completely absent. There is diplopia and dizziness when closing the eye, there is no way to correctly assess the location of the object. In paralytic strabismus, the angle of the primary deviation (squinting eye) is less than the angle of the secondary deviation (healthy eye), that is, when you try to fix the point with the squinting eye, the healthy eye deviates by a much larger angle.
A patient with paralytic strabismus is forced to tilt or turn his head to correct visual impairment. This adaptive mechanism passively transmits the image of an object to the central recess of the retina, which eliminates double vision and provides binocular vision that is not completely perfect. In paralytic strabismus, a forced turn or tilt of the head should be distinguished from the state of torticollis or otitis media.
With damage to the motor nerves of the eye, ptosis of the eyelids, dilated pupil, deviation of the eye outward and downward, partial ophthalmoplegia and paralysis of accommodation occur.
Unlike paralytic strabismus, diplopia is not usually seen with concomitant strabismus. The range of motion of the squinting and fixing eyes is approximately the same and unlimited, the angle of single and secondary deviations is equal, the functions of the motor muscles of the eye are not disturbed. When fixing the gaze on the object, one or, respectively, both eyes deviate in any direction.
Associated strabismus can be horizontal (converging or diverging), vertical (supervergent or infraverging), torsion (cyclotropia), combinative; may be monolateral or alternating.
With monolateral strabismus, the visual function of the squinting eye is suppressed by the central part of the visual analyzer, which is accompanied by a decrease in visual acuity of this eye and the development of dysbinocular amblyopia of varying severity. With alternating strabismus, amblyopia usually does not develop or is mild.



















